March 2024
In this VETgirl online veterinary continuing education blog, we review some common spring plant exposure in dogs and cats. From gastrointestinal to cardiovascular and the central nervous system, we’ll cover a few of the most common plants you should familiarize yourself with, as you’ll see these present to you in the veterinary clinic.
By Dr. Renee Tourdot, DABT, DABVT
When The Best Laid Plants Go Awry: Handling Common Spring Plant Exposures in Dogs and Cats
As the shadows of winter give way to the sunrays of spring, we start to see whispers of green emerge from the earth. Then the dog gets let out, tramples them, rips them out of the ground, and eats them.
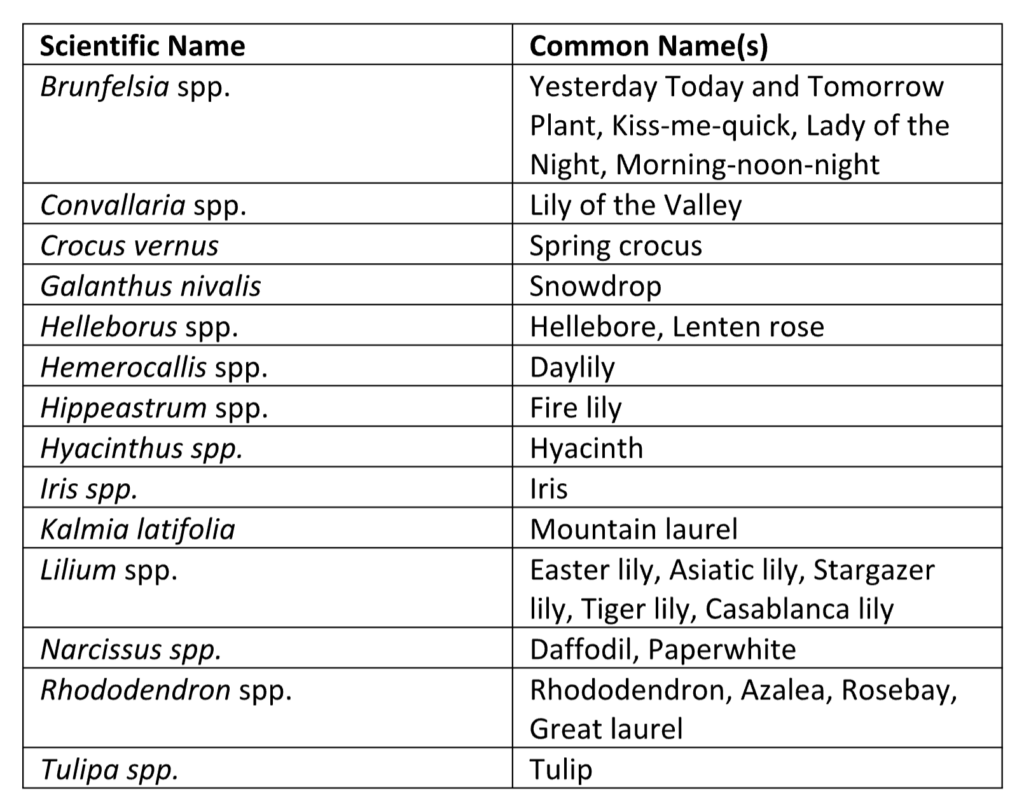
Companion animal exposures to these plants are very common. A basic familiarity with the most common spring-blooming plants is a helpful tool for any veterinary medical professional. It is worth noting that many plants are toxic, however, this does not necessarily mean an exposure is going to be life-threatening. When presented with a patient after a plant exposure, first take a thorough medical and exposure history, perform a physical examination, and then determine the actual risk for the patient before determining what treatments, if any, are indicated. Be sure the plant in question has been properly identified with its scientific name, as many different plants can share a common name, such as “lily.” Assistance with plant identification can be found at community garden centers, poison control hotlines, and reputable social media groups. If the plant in question was part of a home or commercial landscape, then also determine if any fertilizers or pesticides were used alongside it. During the physical examination, be sure to look for evidence of pollen or other plant material on the haircoat, in the teeth, or in the vomitus.
Unfortunately, the question of “how much plant material is too much?” does not come with a standard answer. The answer to this question is complicated by many factors including the time of year, the part of the plant ingested, the health of the plant, the soil quality, the species of animal involved, and knowledge gaps in the scientific literature. If after taking a complete history and performing a physical examination, an accurate risk assessment cannot be determined, it is reasonable to perform decontamination (only if there is minimal risk of doing so) and then to monitor the patient closely for the development of clinical signs.
Plants that Target the Gastrointestinal System
- Ornamental Bulbs and Rhizomes
- Common ornamental bulbs and rhizomes include Crocus spp., Iris spp., Hyacinthus spp., Tulipa spp., Narcissus spp., Clivia spp., Hippeastrum spp., and Galanthus nivalis. These plants contain a variety of alkaloids that irritate the gastrointestinal tract. All parts of the plants are considered toxic, however, the highest concentration of alkaloids is within the bulb. Larger exposures to the toxic alkaloids (primarily bulb ingestion) can cause CNS signs such as depression, ataxia, and tremors. Seizures are rare but possible.1 Ingestion of the densely fibrous bulbs can also cause gastrointestinal obstruction in some patients. In most cases, signs will develop within a few hours. In healthy patients, exposures to plant foliage usually do not require decontamination. The risk is for mild to moderate vomiting, diarrhea, and lethargy. Patients can be monitored for signs and treated symptomatically with antiemetics, fluid therapy, and a bland diet. Exposures to plant bulbs are more likely to result in CNS signs or foreign body obstruction (FBO). In these cases, induction of emesis can be performed. If most or all of the plant material is recovered, then the patient can be given an antiemetic and monitored for ongoing signs. Activated charcoal administration is usually not needed, although if emesis is unsuccessful and bulb material was ingested it could be considered. More severe gastrointestinal signs may require IV fluid therapy, antacids, sucralfate, or exploratory laparotomy for suspected FBO. Mild tremors and seizures can be treated with benzodiazepines while more severe tremoring can be managed with methocarbamol.
- Wisteria spp.
- Wisteria spp. contain lectin (a glycoprotein) and wisterin (a glycoside) in all parts of the plant although they are concentrated in the seeds and pods.2 Ingestion of plant material will usually result in mild to severe gastroenteritis depending on the quantity and parts of plant material ingested. Patients that ingest foliage or flowers can usually be monitored for gastrointestinal signs and treated symptomatically if they develop. Patients that ingest the seed pods can have emesis induced and then be treated with an antiemetic. Rarely, patients may need hospitalized care with IV fluids, antacids, sucralfate, antidiarrheals, and nutritional support.
Plants that target the Cardiovascular System
- Rhododendron spp. and Kalmia spp.
- The primary toxic components of these common ornamental plants are grayanotoxins. Grayanotoxins are found in all parts of the plant including the nectar, which means that honey derived from these plants can also be toxic. Grayanotoxins bind and slow down the opening and closing of sodium channels, resulting in more persistent depolarization. Thus, the excitable membranes of myocytes and neurons are most sensitive to these
toxins.3 Affected patients will usually develop hypersalivation and/or vomiting within 30 minutes. Bradycardia, hypotension, lethargy, weakness, ataxia, disorientation or agitation, tremors, and dyspnea may occur within 6 hours.4 Signs may last 24 – 72 hours. Decontamination by induction of emesis and/or administration of activated charcoal is recommended if more than a mouthful of plant material is ingested. An antiemetic can be administered, and patients should then be monitored closely for development of further signs and treated symptomatically. If cardiovascular signs develop, the patient should be started on non-calcium-containing IV fluid therapy and serum potassium should be monitored as hypokalemia can exacerbate signs. Atropine can be given as needed for bradycardia. Benzodiazepines can be used for tremors or seizures (rare).
- The primary toxic components of these common ornamental plants are grayanotoxins. Grayanotoxins are found in all parts of the plant including the nectar, which means that honey derived from these plants can also be toxic. Grayanotoxins bind and slow down the opening and closing of sodium channels, resulting in more persistent depolarization. Thus, the excitable membranes of myocytes and neurons are most sensitive to these
- Helleborus spp. and Convallaria spp.
- Hellebore are popular perennials that bloom in very early spring. They contain protoanemonin and saponins that serve to irritate the gastrointestinal mucosa. Vomiting, diarrhea, anorexia, and colic are common. More concerningly, these plants contain bufadienolides, which are digitalis-like glycosides (cardenolides).5
- Convallaria spp. contain a vast array of potent cardenolides. Similar to Helleborus spp., initial signs are usually gastrointestinal in nature but can quickly progress to cardiovascular instability. For both Helleborus spp. and Convallaria spp., all parts of the plant are toxic, but the roots and rhizomes are the most toxic.6 Cardenolides inhibit the sodium-potassium-ATPase pump on cell membranes. This results in increased intracellular sodium. Excess sodium ions are exchanged for calcium via the sodium-calcium exchanger. The resultant increase in intracellular calcium slows conduction and increases contractility.7 Patients typically develop bradyarrthymias and hypotension. Hyperkalemia, tachyarrhythmias and ventricular fibrillation are also possible. Signs typically start within 24 hours of exposure although they may be delayed out to 3 days. GI signs are usually seen first. When appropriate, patients ingesting more than a mouthful of these plants can have emesis induced. An antiemetic can then be administered. If emesis is unsuccessful or only partially successful, a single dose of activated charcoal can be administered. Patients should be monitored for a minimum of 24 hours for the development of cardiovascular signs. For exposures to large amounts of plant material, continuous ECG monitoring is ideal. If cardiovascular signs develop, serum potassium levels should be monitored closely. The patient can be started on non-calcium-containing IV fluids. Atropine or glycopyrrolate can be used for bradyarrhythmias. Ventricular arrhythmias can be treated with lidocaine or phenytoin. Insulin and dextrose are recommended for severe hyperkalemia. Refractory arrhythmias can be treated with digoxin immune Fab (Digibind®), a digoxin-specific antibody derived from immunized sheep, that works rapidly and can be life-saving in the most severe cases.8
Plants that target the Central Nervous System
- Brunfelsia spp.
- Brunfelsia spp. are common ornamental shrubs found in the southern United States. They contain several potent compounds that contribute to their toxicity. Most notably is brunfelsamidine, which causes tremors and seizures.9 Affected patients typically display vomiting, diarrhea, ataxia, tremors, and seizures. Cardiac arrhythmias are also possible.10 Patients may appear hyperesthetic, disoriented or agitated. Severely affected patients may suffer hyperthermia, DIC, rhabdomyolysis, and death. Any exposed patient should be evaluated and treated. Patients will show signs within 12 hours of exposure. Decontamination must be approached with caution, as neurologic patients are at increased risk of suffering complications such as aspiration pneumonia. If a large amount of plant material was ingested and the patient is already neurologic, intubation and administration of a single dose of activated charcoal with sorbitol via orogastric tube can be considered. Gastric lavage could also be attempted, but recovery of plant material may be limited. Serial water enemas every 6-8 hours may also help hasten the elimination of plant material. Tremors can be controlled with methocarbamol and seizures may be controlled with benzodiazepines, levetiracetam, or phenobarbital. The patient should be placed on an intravenous balanced crystalloid fluid and monitored closely for complications such as hyperthermia, rhabdomyolysis, acidosis, and DIC. Severe signs may last several days with minor tremors potentially continuing for several weeks.
Plants that target the Kidneys
- Lilium spp. and Hemerocallis spp.
-
- Although these plants typically won’t bloom until summer in most climates, we do start to see Lilium spp. (particularly the Easter lily, Lilium longiflorum) in spring floral arrangements. Much of what makes these plants particularly toxic remains a mystery although the toxin appears to be water-soluble.11 Cats are the only species known to exhibit signs of toxicity. Clinical signs manifest initially as vomiting and lethargy. Within 48 hours, signs can progress to anorexia, polyuria, polydipsia, acute kidney injury, oliguria or anuria, and death. Any exposure, including dermal exposures to pollen, should be considered to put the patient at risk of AKI. If a large amount of plant material was ingested, then emesis can be induced. If there was a dermal exposure, then the patient should be bathed with mild dish soap. The patient should be then placed on a diuretic rate of an intravenous balanced crystalloid fluid for 48 hours. Renal function should be monitored closely, and any signs may be treated symptomatically. Patients that receive prompt fluid diuresis have an excellent prognosis.12 Patients whose treatment is delayed or who develop oliguria have a poor prognosis.
-
References:
1. Lieske CL. Spring-blooming bulbs: A year-round problem. In: Veterinary Medicine. August 2002: pp 580-588.
2. Burrows GE, Tyrl RJ. Toxic Plants of North America 2nd ed. 2013. John Wiley & Sons Inc. pp 629.
3. Burrows GE, Tyrl RJ. Toxic Plants of North America 2nd ed, 2013. John Wiley & Sons Inc. pp 437.
4. Manhart IO, DeClementi C, Guenther CL. Mountain laurel toxicosis in a dog. J Vet Emerg Crit Care 2013;23(1):77-81.
5. Burrows GE, Tyrl RJ. Toxic Plants of North America 2nd ed, 2013. John Wiley & Sons Inc. pp 1014
6. Burrows GE, Tyrl RJ. Toxic Plants of North America 2nd ed, 2013. John Wiley & Sons Inc. pp 763-764.
7. Galey FD. “Cardiac Glycosides” In Clinical Veterinary Toxicology, edited by Konnie H Plumlee, 386-387. Mosby Inc,
2004.
8. Zoltani CK. “Cardiovascular Toxicity” In Veterinary Toxicology, 3rd ed, Edited by Ramesh C. Gupta, 229. Elsevier Inc. 2018.
9. Burrows GE, Tyrl RJ. Toxic Plants of North America 2nd ed. 2013. John Wiley & Sons Inc. pp 1135.
10. Clipsham R. Brunfelisa australis (Yesterday, Today, And tomorrow Tree) and Solanum Poisoning in a Dog. J Am Anim Hosp Assoc 2012;48:139-144.
11. Rumbeiha WK, Francis JA et al. A comprehensive study of Easter lily poisoning in cats. J Vet Diagn Invest 2004;
16:527-541.
12. Bennett AJ, Reineke EL. Outcome following gastrointestinal tract decontamination and intravenous fluid diuresis
in cats with known lily ingestion: 25 cases (2001-2010). J Am.Vet Med Assoc 2013; 242:1110-1116.
Only VETgirl members can leave comments. Sign In or Join VETgirl now!



Is there any real data on Hemerocallis toxicity? I have never seen a daylily toxicity in cats only the Lilium family. There seems to be quite a bit of confusion on this topic. Daylily flowers are not toxic to deer that is for sure!
This is a great blog to keep referencing back to!