VETgirl® Website Terms and Conditions
Thank you for visiting the website of VETgirl (“VETgirl”). These Terms and Conditions (the “Terms and Conditions”) apply to the VETgirl website (https://vetgirlontherun.com) and include, without limitation, related mobile websites, microsites, mobile applications, VETgirl profiles on social media sites and any other digital services or properties operated or used by VETgirl (collectively referred to as the “Sites”). By using the Sites, you agree to comply with and be bound by these Terms and Conditions and VETgirl’s Privacy Policy. Please read these Terms and Conditions and the Privacy Policy carefully. By subscribing to be a VETgirl member, you are also agreeing to our Subscription Agreement found HERE. If you do not agree to both these Terms and Conditions and the Privacy Policy, you must immediately terminate your use of the Sites.
1. License. We grant you a nonexclusive nontransferable license to use the Sites and the services therein subject to the terms hereof for a period beginning on the date of acceptance of these Terms and Conditions and ending on the earlier of: (a) the date we notify you of our termination of these Terms and Conditions; or (b) the date you notify us of your termination of these Terms and Conditions. It is your responsibility to properly protect your login information, including your username and password, from use by third parties. Licenses for viewing any Continuing Education (“CE”) program and listening to podcasts will be subject to the terms of the applicable subscription or one-time purchase. You may use the Sites and VETgirl Content (as defined below, see Section 6) for your noncommercial personal use and for no other purpose. Sharing of accounts is against the TOS and subject to immediate cancellation of account without refund. Individual accounts are for that individual only. TEAM VETgirl accounts, while cost-effective, are also for individual use only. When creating a team account, each individual within that team is provided with an individual account for website access which can not be shared nor transferred to another individual.
2. License Restrictions. Unless otherwise expressly stated in these Terms and Conditions or you receive VETgirl’s prior written consent, you may not modify, translate, create derivative works of, copy, distribute, market, display, remove or alter any proprietary notices or labels from, lease, sell, sublicense, clone, transfer, decompile, reverse engineer, or incorporate into any information retrieval system (electronic or mechanical), the Sites, any VETgirl Content (as defined below, Section 6), or any portion thereof. Further, you may not: (a) use the Sites for any unauthorized or illegal purpose or activity including, but not limited to, any activity to obtain or attempt to obtain unauthorized access to the Sites, including VETgirl Content; (b) interfere with the proper working of the Sites including, but not limited to, the transmission of any virus, worm, trap door, back door, timer, clock, Trojan horse, denial of service attack or other limiting routine, instruction or design; or (c) interfere with any other person’s use and enjoyment of the Sites.
3. Your Acceptance; Revisions to Terms and Conditions. The Sites are available only to individuals who can enter into legally binding contracts under applicable law. These Terms and Conditions constitute a legally binding agreement between you and VETgirl regarding your use and access to the Sites. By using the Sites you unconditionally agree to these Terms and Conditions. VETgirl reserves the right to revise these Terms and Conditions at any time in its sole discretion by posting revised Terms and Conditions to the Sites. Your use of the Sites signifies your acceptance of all the terms of use contained within the Terms and Conditions posted at the time of your use.
4. Privacy Policy. For information about VETgirl’s data protection practices and VETgirl’s use and protection of your personal information, please read VETgirl’s Privacy Policy which is incorporated by reference into these Terms and Conditions.
5. User Obligations. As a precondition to use the Sites, you warrant and guarantee that you will abide by, without limitation, all applicable local, state, national and international laws and regulations with respect to your use of the Sites and not interfere with the use and enjoyment of the Sites by other users or interfere with VETgirl’s operation and management of the Sites. You unconditionally agree that you will not use the Sites to upload, download, post, email, transmit or otherwise make available any Content, including through any attachments thereto:
(a) that is unlawful, harmful, threatening, abusive, harassing, tortious, defamatory, vulgar, obscene, libelous, invasive of another’s privacy, hateful, or racially, ethnically or otherwise objectionable;
(b) that you do not have a right to make available under any law or under contractual or fiduciary relationships (such as, but not limited to, inside information, proprietary and confidential information learned or disclosed as part of employment relationships or under nondisclosure agreements);
(c) that infringes any patent, trademark, trade secret, copyright or other proprietary rights of any party;
(d) any unsolicited or unauthorized advertising, promotional materials or spam;
(e) any material that contains software viruses or any other computer code, files or programs designed to interrupt, destroy or limit the functionality of any computer software or hardware or telecommunications equipment; and
(f) that may intentionally or unintentionally violate any applicable local, state, national or international law.
6. Trademarks and Copyrights: Content. The Content of the Sites includes, without limitation,
(a) VETgirl’s trademarks, service marks, logos, brands, and brand names, trade dress and trade names and other distinctive identification (collectively “VETgirl Marks”);
(b) information, data, materials, interfaces, computer code, databases, products, services, software applications and tools, text, images, and photographs; and
(c) the design, structure, selection, compilation, assembly, coordination, expression, functionalities, applications, look and feel, and arrangement of any content contained in or available through the Sites (the items identified in subsections (a) (b) and (c) shall be collectively referred to herein as “VETgirl Content” or “Content”).
VETgirl Content is the property of VETgirl, its licensors, sponsors, partners, advertisers, content providers or other third parties and is protected by law. The reproduction, transmission, distribution, sale, publication, broadcast, circulation or dissemination of any VETgirl Content by you, or by you through any other person or entity, is strictly prohibited and unlawful unless express written consent is separately obtained from the owner of such Content. You may not alter, delete, obscure or conceal any copyright or other notices appearing in any VETgirl Content.
7. No Reproduction or Resale. You are not authorized to use any intellectual property owned by VETgirl for resale to any other person or entity. You may not modify, copy, distribute, transmit, display, perform, reproduce, publish, license, create derivative works from, transfer, or sell any intellectual property, information, software, products, or services obtained from the Sites. You may, however, stream or download, where specifically permitted, podcasts, videos and/or related materials from the Sites for your personal, educational, non-commercial use only, provided you keep intact all copyright, trademark, and other proprietary notices.
8. No Unlawful, Prohibited, or Reckless Use. As a condition of your use of the Sites and the services and products therein, you warrant to VETgirl that you will not use the Sites for any purpose that is unlawful or prohibited by these Terms and Conditions. You may not use the Sites in any manner that could jeopardize your safety or the safety of others, including texting, streaming, e-mailing, or using the Sites while driving, running, or participating in other activities that require your attention to safety.
9. Notification of Claimed Copyright Infringement. Pursuant to 17 U.S.C. Section 512(c)(2) of the Copyright Act, VETgirl designates the following individual as its agent for receipt of notifications of claimed copyright infringement:
Name: Dr. Garret Pachtinger
Title: Program Director, Educational Services
Phone Number: 858-859-1838
Email: [email protected]
Address available upon request
10. Third Party Information, Advertisements and Websites: Exclusion of Liability. Use of the Internet and the Sites is solely at your risk and is subject to, without limitation, all applicable local, state, national and international laws and regulations. Unless expressly required by law, VETgirl does not and cannot guarantee the confidentiality or security of any communication or other material transmitted to or from the Sites over the Internet or other communication networks. The Sites may contain advertisements, but the inclusion of advertisements on the Sites does not imply endorsement of the advertised products or services. VETgirl shall not be responsible for any loss or damage of any kind incurred as a result of the presence of such advertisements on the Sites. The Sites also may feature materials, information, products, and services provided by third parties. Any such information, including but not limited to articles, opinions, advice, statements, services, offers or other information made available by third parties such as content providers and other users of the Sites are those of the respective third party and not of VETgirl or its affiliates. VETgirl makes no representation with respect to, nor does it guarantee or endorse, the quality, non-infringement, accuracy, completeness, timeliness, or reliability of such third-party materials, information, services or products. Please note that some of the links listed on this site may contain affiliate links.
11. Indemnification. If anyone brings a claim or threatened claim against VETgirl arising out of your actions or use of the Sites or the services and products therein, or anyone else’s use thereof through your account, you agree to indemnify and hold VETgirl, its parents, subsidiaries, affiliates, managers, officers, agents, independent contractors, and employees harmless from any claim or demand, including reasonable attorney’s fees and costs at arbitration, through trial or on appeal, in addition to all other sums provided by law.
12. DISCLAIMER OF WARRANTIES. THE SITES, INCLUDING SERVICES AND PRODUCTS ON THE SITES, ARE PROVIDED ON AN “AS IS” AND “AS AVAILABLE” BASIS AND WITHOUT ANY WARRANTIES, EXPRESS OR IMPLIED. YOUR USE OF THE SITES, INCLUDING ITS SERVICES AND PRODUCTS, IS AT YOUR OWN RISK. VETGIRL DISCLAIMS ALL WARRANTIES regarding the accuracy, safety, and/or completeness of the information contained IN THE SITES. TO THE FULLEST EXTENT PERMITTED BY APPLICABLE LAW, VETGIRL DISCLAIMS ANY AND ALL REPRESENTATIONS AND WARRANTIES OF ANY KIND, EXPRESS OR IMPLIED, INCLUDING BUT NOT LIMITED TO THE IMPLIED WARRANTIES OF MERCHANTABILITY AND FITNESS FOR A PARTICULAR PURPOSE, AND NONINFRINGEMENT. WHILE WE TAKE REASONABLE PRECAUTIONS AGAINST INFECTION OF THE SITES BY MALWARE, WE CANNOT GUARANTEE THERE WILL BE NO SUCH INFECTION. NOR CAN WE GUARANTEE THAT THE SITES WILL BE PROVIDED IN A MANNER THAT IS UNINTERRUPTED, TIMELY, SECURE OR ERROR-FREE. SOME JURISDICTIONS DO NOT ALLOW THE EXCLUSION OF IMPLIED WARRANTIES; THEREFORE, THE ABOVE-REFERENCED EXCLUSION IS INAPPLICABLE IN SUCH JURISDICTIONS. The SITES AND THE SERVICES AND PRODUCTS THEREIN are intended for THE EDUCATION OF veterinary professionals only and are not intended to be a substitute for professional veterinary advice, diagnosis, or treatment. These materials are intended to provide information for educational purposes only AND ARE THE INTERPRETATIONS OF VETGIRL AND/OR ITS DIRECTORS, OFFICERS, MANAGERS, EMPLOYEES, INDEPENDENT CONTRACTORS, AND AGENTS. You should not rely on information from The SITES AND THE SERVICES AND PRODUCTS THEREIN in place of PEFORMING YOUR OWN MEDICAL RESEARCH, VERIFYING ALL INFORMATION AGAINST VETERINARY LITERATURE, AND/OR seeking professional advice and assistance. YOU are responsible for confirming all medical information such as drug doses and medical accuracy against veterinary literature as needed.
13. LIMITATION OF LIABILITY. WE DO NOT GUARANTEE THAT THE SITES WILL ALWAYS BE SAFE, SECURE OR ERROR-FREE OR THAT THE SITES WILL ALWAYS FUNCTION WITHOUT DISRUPTIONS, DELAYS OR IMPERFECTIONS. VETGIRL IS NOT RESPONSIBLE FOR THE ACTIONS, CONTENT, INFORMATION, OR DATA OF THIRD PARTIES, AND YOU RELEASE US, OUR DIRECTORS, OFFICERS, MANAGERS, EMPLOYEES, INDEPENDENT CONTRACTORS, AND AGENTS FROM ANY CLAIMS AND DAMAGES, WHETHER IN CONTRACT, TORT (INCLUDING NEGLIGENCE), KNOWN AND UNKNOWN, ARISING OUT OF OR IN ANY WAY CONNECTED WITH ANY CLAIM YOU HAVE AGAINST ANY SUCH THIRD PARTIES. IF YOU ARE A CALIFORNIA RESIDENT, YOU WAIVE CALIFORNIA CIVIL CODE §1542, WHICH SAYS: A GENERAL RELEASE DOES NOT EXTEND TO CLAIMS WHICH THE CREDITOR DOES NOT KNOW OR SUSPECT TO EXIST IN HIS FAVOR AT THE TIME OF EXECUTING THE RELEASE, WHICH IF KNOWN BY HIM MUST HAVE MATERIALLY AFFECTED HIS SETTLEMENT WITH THE DEBTOR. WE WILL NOT BE LIABLE TO YOU FOR ANY LOST PROFITS OR OTHER CONSEQUENTIAL, SPECIAL, INDIRECT, OR INCIDENTAL DAMAGES ARISING OUT OF OR IN CONNECTION WITH THESE TERMS AND CONDITIONS OR THE SITES, EVEN IF YOU HAVE BEEN ADVISED OF THE POSSIBILITY OF SUCH DAMAGES. YOU AGREE THAT OUR AGGREGATE LIABILITY ARISING OUT OF THESE TERMS AND CONDITIONS, THE SITES AND YOUR USE OF THEM, OR THE SERVICES AND PRODUCTS THEREIN WILL NOT EXCEED THE GREATER OF ONE HUNDRED DOLLARS ($269) OR THE AMOUNT YOU HAVE PAID US IN THE PAST TWELVE (12) MONTHS. Any claims arising in connection with your use of the SITESAND any Content THEREIN must be brought within one (1) year of the date of the event giving rise to such action occurred. APPLICABLE LAW MAY NOT ALLOW THE LIMITATION OR EXCLUSION OF LIABILITY OR INCIDENTAL OR CONSEQUENTIAL DAMAGES, SO THE ABOVE LIMITATION OR EXCLUSION MAY NOT APPLY TO YOU. IN SUCH CASES, VETGIRL’S LIABILITY WILL BE LIMITED TO THE FULLEST EXTENT PERMITTED BY APPLICABLE LAW. YOU ARE SOLELY RESPONSIBLE FOR ANY DAMAGE TO YOUR COMPUTER SYSTEM OR LOSS OF DATA RESULTING FROM YOUR USE OF THE SITES AND ANY VETGIRL SERVICES AND PRODUCTS.
14. Termination. VETgirl may terminate your account, and remove and discard any of your content, at any time without notice, for any reason. We will not be liable to you or any third-party for any termination of your access to the Sites. You may also delete or disable your account at any time.
15. Choice of Law and Exclusive Venue. You agree that all disputes arising under or related to your use or access of the Sites, the products and services offered therein, and these Terms and Conditions shall be brought solely in the federal and state courts situated in the County of Hillsborough, State of Florida. You consent to personal jurisdiction and venue in the federal and state courts situated in the County of Hillsborough, State of Florida. The validity, interpretation, construction, performance, enforcement, remedies, and the rights and obligations of the parties to the Sites, the products and services offered therein, and these Terms and Conditions, shall be governed and construed by the substantive laws of the State of Florida (without regard to the conflict of laws rules or statutes of Florida or any other jurisdiction that might result in the application of other law).
16. Entire Agreement. These Terms and Conditions, along with the VETgirl Privacy Policy, constitute the entire agreement between you and VETgirl with respect to the subject matter herein and supersedes all prior oral and written agreements, promises, negotiations, commitments, representations, inducements, statements and communications. No oral representation and no prior or contemporaneous oral or written matters extrinsic to these Terms and Conditions shall have any force or effect as to the provisions of these Terms and Conditions. All prior and contemporaneous discussions concerning the subject matter of these Terms and Conditions have been merged and integrated into, and are superseded by, these Terms and Conditions.
17. Modifications and Amendments. VETgirl reserves the right, at any time, to modify or amend the Terms and Conditions without prior notice to you. Modifications and/or amendments are effective immediately upon being posted on the Sites. Your continued use of the Sites and the services and products therein after any modifications or amendments are posted constitutes your acceptance of the modifications or amendments. Except as provided in this paragraph, these Terms and Conditions may not be amended except by agreement in writing signed by the party against whom enforcement of the amendment is sought.
18. Waiver. VETgirl’s failure to exercise or enforce any term in these Terms and Conditions will not constitute a waiver of such term.
19. Severability. If any provision of these Terms and Conditions is declared to be invalid, unenforceable, or void by a court of competent jurisdiction, such provision will be deemed stricken, and the Terms and Conditions will be reformed to replace that provision with a valid and enforceable provision which comes as close as possible to expressing the intention of the stricken provision. The remainder of the Terms and Conditions shall have the same force and effect as if such provision had never been included.
20. Attorney’s Fees. In the event that any action, suit or legal proceeding is initiated or brought to enforce any or all of the provisions of these Terms and Conditions, you agree that VETgirl shall be entitled, in addition to any other remedies provided by law or equity, to collect from you, and you agree to pay VETgirl its costs and expenses, including reasonable attorney’s fees, costs, disbursements, photocopy charges, witness fees, subpoena fees, expert witness fees, computerized legal research fees, computer forensics consulting fees, and all other expenses incurred by VETgirl, including those on appeal and in connection with the enforcement or collection of any order, award, or judgment against you, to the extent that VETgirl prevails (in whole or part) in such legal proceeding.
21. Assignability. The rights, responsibilities, or obligations granted or assumed with respect to these Terms and Conditions and any subscription or CE purchased by you through the Sites may not be assigned by you, in whole or in part, without first obtaining VETgirl’s written consent.
22. Rule of Construction. It is expressly agreed by the parties to these Terms and Conditions that the rule of construction that a document should be more strictly interpreted against the person who drafted it shall not apply to any provision.
23. Use of Websites and Content outside of the United States. VETgirl makes no claims regarding access or use of the Sites or the VETgirl Content outside of the United States. If you use or access the Sites or the VETgirl Content outside of the United States, you do so at your own risk and are responsible for compliance with the laws of your jurisdiction as well as these Terms and Conditions.
24. Continuing Education Programs. All CE programs offered on the VETgirl website are certified by the Registry of Approved Continuing Education (“RACE”). VETgirl cannot guarantee your satisfactory completion of any CE course or that you will be granted CE credit for having completed a course. It is your responsibility to verify and track its CE completion status and eligibility for credit. Typically, a certificate for completion of CE programs will be provided to you if you attended a live, interactive CE webinar for the complete duration of the webinar or (a) successfully complete an online quiz for each CE program (with a score of at least 80% correct); and (b) certify that you are the person who actually took the quiz.
25. Verification of Medical Information and Course Qualification. It is your responsibility to verify that any CE course completed through the Sites qualifies for CE credit in your state. While we believe that the information contained in the Sites and any CE course offered through the Sites is accurate at the time it is posted to the Sites, there are frequently new scientific discoveries and changes to accepted veterinary practices. Likewise, the some of the Content may be the expressed scientific and medical opinion of the speaker. It is your responsibility to verify that the information provided is still accurate and up-to-date. We make no guarantee that your use of the information or techniques contained in or demonstrated in any CE course offered through the Sites will be successful. Further, reviewing of CE program materials is not a substitute for all aspects of in-person training, where the trainer is able to evaluate your skills in using the techniques demonstrated. You are responsible for confirming all medical information such as drug doses and medical accuracy against veterinary literature as needed.
26. Social Media. VETgirl may provide opportunities for user interaction within its Sites and social media profiles on sites such as Facebook, Twitter, LinkedIn, and various blogging sites. On those social media profiles, content and links to other Internet sites should not be construed as an endorsement of the organizations, entities, views or content contained therein. VETgirl is not responsible for content or links posted by others. Also note that any links on our website do not imply any sort of endorsement. Please note that you are using these links at your own risk.
27. User-Generated Content. By contributing user-generated Content to any of the Sites or social media profiles, you acknowledge that this information is available to the public and grant VETgirl a nonexclusive license to display, reproduce, transmit, modify such user-generated Content and that VETgirl may use the user-generated Content for internal and external marketing purposes. You are solely responsible for the user-generated Content you submit. VETgirl retains the right to remove any Content from the Sites for any reason.
28. Membership Renewal Our continuous service program takes all the hassle out of renewing your subscription. It avoids service interruption by automatically renewing your subscription at the best available rate. Your renewal will guarantee uninterrupted service until the new expiration date of your renewed subscription. If the user would like to cancel their renewal, they must do so within their account dashboard. Please review our help center page here for more information.
© 2021 VETgirl. All rights reserved.
This document was last updated on May 17, 2021.
_______________
Thank you for this description. Good points to remember. I especially find the levels of alertness helpful. Sometimes BAR vs. QAR just doesn’t explain it all.
When you describe perfusion and O2 saturation being variable based on mm color, how accurate is a pulse oximeter on something that has a grey color? We recently had a dog with labored breathing, grey mm that had a pulse ox reading of 97%. Just curious on your thoughts there.
It’s typically due to poor perfusion – their hemoglobin can still carry oxygen, but they may be shocky and poorly perfused.
Makes sense. I think labored breathing resulting in a cyanotic patient with blue mm would read low oxygen saturation, but grey gums, probably increased CRT too, indicate inadequate peripheral infusion, which wouldn’t necessarily read any more abnormal then 97% which is abnormal to begin with. I think your patient probably anemic and dehydrated (maybe a parasite infection, hemorrhaging, Parvo etc). So those decreased RBCs could be functioning normally, I.e. hemoglobin were still carrying enough O2, for the moment!. Pulse Ox can be so finicky. For me, an EKG and a Parks Doppler combo beat pulseOx. Their just never 100% right 100% of the time.
Sorry perfusion , not infusion
Perfusion
I just have to share this story. I’m a vet and used to take emergencies after hours. I asked a few questions similar to what you have in order to assess the urgency of the call. I’ll never forget the client who responded to my first few questions by saying- “I know my dog is still alive! I can see his brain beating!”
Oh my. Where do you go with that?
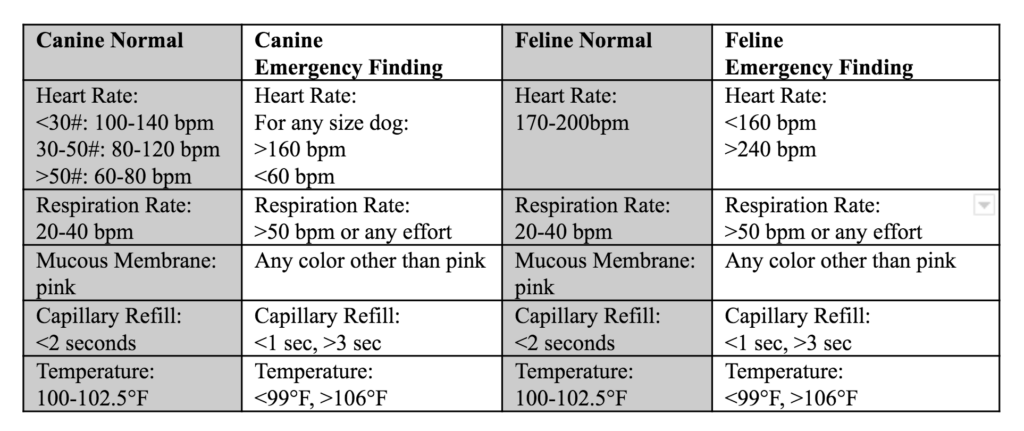
Can you tell me the reference you used for your chart? It is a great source for weight breakdowns for dogs.
Posting the table is an excellent idea.
Good triage skills to know.
These were very helpful key points.
I am a credentialed veterinary technician who works overnights as a patient care tech, usually without a veterinarian present.These key points are extremely important for us technicians when we need to call the DOD. Most of us do not wait till we are asked, how RR, HR, temp, MM/CRT are. That is part of the beginning of the conversation, right after which patient it is. Great refresher for those who may need it.
Good Reminders