April 2024
By Chelsea Camiolo, BS, CVT, VTS (SAIM), BluePearl (Internal Medicine)
Hyperadrenocorticism: Easy to Spot, Harder to Diagnose
In this VETgirl online veterinary continuing education blog, we take the mystery out of how to diagnose Cushing’s disease. Everyone knows the classic signs of Cushing’s disease: panting, PU/PD, potbelly appearance, thin skin, and hair loss. But which test is better to diagnose it? How are these tests performed? What monitoring is suggested once treatment is initiated? Read on as Chelsea answers these common veterinary diagnostic questions associated with Cushing’s disease.
It is important to have a strong suspicion of Cushing’s disease before testing for it. It is also important to consider the patient’s temperament before choosing what diagnostic test to start with. None of these tests are 100% accurate, and results may be affected by illness or stress.
Once a patient has presented with strong clinical signs suggestive of Cushing’s disease, typically, the first step is running routine bloodwork, including a complete blood count, chemistry panel, and urinalysis.
Excessive secretion of glucocorticoids typically results in a “stress leukogram” characterized by lymphopenia, eosinopenia, neutrophilia, and monocytosis.1 Any sick dog can exhibit a stress leukogram, so that alone isn’t diagnostic for Cushing’s disease. An increase in alkaline phosphatase (ALP) activity is noted in 85-90% of dogs with hyperadrenocorticism.1 Dogs with Cushing’s disease may also exhibit mild hyperglycemia, as well as a potential urinary tract infection due to the immunosuppression from the excess glucocorticoids in their system. These patients will also have a urine specific gravity of less than 1.020 in most cases, and proteinuria.
Based on these results, the next step would be to pursue diagnostic testing specific to Cushing’s disease. There are multiple options, including urine cortisol:creatinine ratio, adrenocorticotropic hormone (ACTH) stimulation test, low-dose dexamethasone suppression test, high-dose dexamethasone suppression test, and endogenous ACTH. The low-dose dexamethasone suppression test (LDDST) is the screening test of choice for spontaneous Cushing’s syndrome in patients without concurrent illness. In patients with nonadrenal illnesses, such as diabetes mellitus, or suspicion of iatrogenic Cushing’s syndrome, an ACTH stimulation test is preferred.2
There are three types of hyperadrenocorticism. The first is pituitary-dependent hyperadrenocorticism (PDH), in which the pituitary gland has a tumor that continuously produces ACTH no matter how much cortisol is present, thereby disrupting the negative feedback loop. The second is a functional adrenal tumor (FAT), in which a tumor on the adrenal gland releases excessive amounts of cortisol, causing the pituitary gland to stop producing ACTH, resulting in a low concentration of ACTH. PDH accounts for 80-85% of cases of hyperadrenocorticism, 15-20% of which are FAT. The third type of hyperadrenocorticism is iatrogenic hyperadrenocorticism, which occurs secondary to the administration of glucocorticoids. An ACTH stim test will differentiate between Addison’s disease, Cushing’s disease, and Iatrogenic Cushing’s disease but cannot distinguish PDH from FAT. An LDDST can, in most cases, differentiate between PDH and FAT, but in some cases a high-dose dexamethasone test may be necessary.
Urine Cortisol:Creatinine Ratio
This test is extremely useful in ruling out Cushing’s disease but is not specific enough to use as a diagnostic test. This test is performed by collecting a free catch urine sample, typically the first urine in the morning, and sending it to the lab to be evaluated. If the patient is under any amount of stress, it will show an elevated cortisol in the urine. Therefore, the urine sample cannot be collected at the veterinary clinic, where stress levels are typically at their highest. This test has a high sensitivity (100%) but a low specificity (22%); thus, a normal UC:CR test (<10) rules out Cushing’s disease, but a high UC:CR cannot be used to confirm the diagnosis of Cushing’s disease.1
Adrenocorticotropic Hormone (ACTH) Stimulation Test
ACTH is a hormone that is naturally produced in a healthy animal’s body. The pituitary-adrenal axis works as a negative feedback loop. ACTH is produced by the pituitary gland, which then tells the adrenal glands to release cortisol. Once the body has enough cortisol in its blood, this enacts the negative feedback on the pituitary gland to stop producing ACTH.
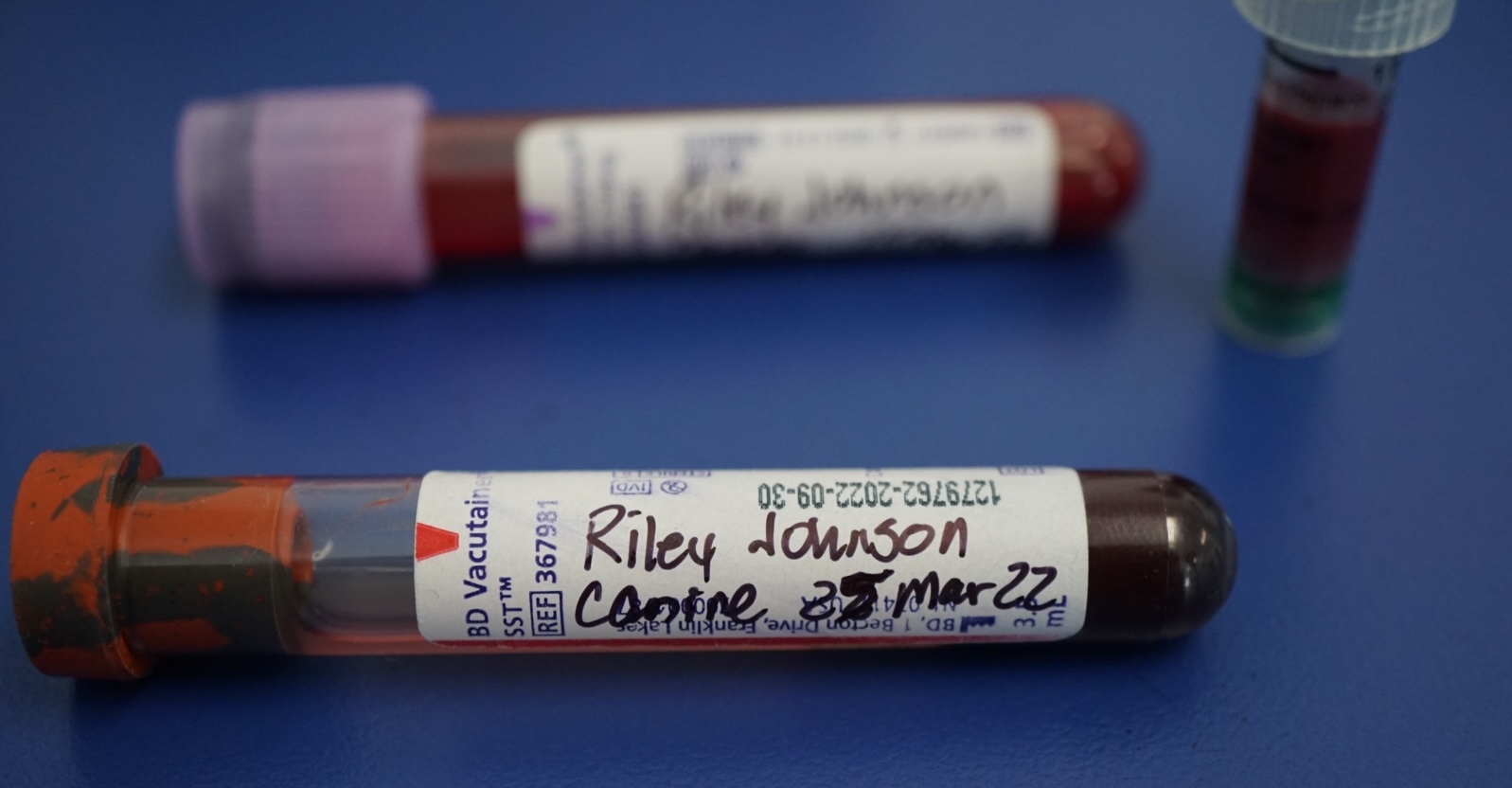
When performing an ACTH stim, you are administering synthetic ACTH, and then measuring the levels of cortisol in the blood. The synthetic ACTH (Cortrosyn™) is given at 5mcg/kg IV. Originally, patients received a full 1 vial (250 mcg), but due to cost and availability, the dose was modified to 5 mcg/kg IV. Because of this, if the first dose is accidentally administered outside of the vein, the dose can be repeated. A serum separator tube sample is collected before administering Cortrosyn™, then again 1 hour after the patient receives the Cortrosyn™. Icterus and lipemia can affect the results, so it is recommended to have patients fasted before performing this test. This can be difficult in diabetic patients, in which case it is at the doctor’s discretion.
If the cortisol levels are both <1 mcg/dL, meaning the adrenal glands released no cortisol in response to the ACTH that was administered, it is diagnostic for hypoadrenocorticism, also known as Addison’s disease. Post-ACTH results greater than 22 mcg/dL are diagnostic for Cushing’s disease.3 If the patient has iatrogenic Cushing’s disease, the pre-sample will typically be between 1-5 mcg/dL, with little to no increase in the post-sample. Disadvantages of this test include the fact that there is a large gray zone of 6-22 ug/dL, meaning if the results fall within that area, there is still a chance these patients have Cushing’s disease. Since this test can be affected by stress, it is difficult to determine if results indicate the patient is heading towards becoming cushingoid, or if they were just stressed that day. ACTH stimulation tests have a sensitivity of 60-85%, and a specificity of 85-90%, and this test lacks sensitivity in dogs with adrenal tumors, resulting in a false negative in 41% of cases.3 While an ACTH stim can be affected by stress, it is less affected than an LDDST. It is also less affected by concurrent illnesses, which makes it a better option for patients with diabetes mellitus. An ACTH stim should also be considered if the LDDST comes back negative, but Cushing’s disease is still strongly suspected, and vice versa. An LDDST should be performed if iatrogenic Cushing’s disease has been ruled out.
Low-Dose Dexamethasone Suppression Test
The LDDST evaluates the negative feedback loop of the hypothalamic-pituitary-adrenal axis (HPAA).1 Dexamethasone is given IV at a dose of 0.01mg/kg. This dose cannot be repeated if it is administered outside of the vein, as it can affect the results. Serum separator samples are collected prior to administering the dexamethasone and then at 4 and 8 hours post dexamethasone. This test has a sensitivity of 90-95% in dogs with PDH and approximately 100% in those with FATs. However, as other diseases can affect the HPAA, the specificity is low at 40-50%.1 This test is highly affected by stress and concurrent illness, leading to a high rate of false positives. Because of this, high-stress patients should first be tested using an ACTH stim. Fasting is not necessary; however, lipemia may affect the results.3
In normal dogs, administering dexamethasone should suppress the secretion of ACTH from the pituitary glands, causing the cortisol concentration to decrease to less than 1.4 mcg/dL 8 hours post-administration.1 In dogs with Cushing’s disease, the administration of dexamethasone will have a minimal effect, and the cortisol concentrations will remain elevated. An 8-hour sample that is >1.4 mcg/dL is consistent with the diagnosis of hyperadrenocorticism, and you can proceed with the differentiation of PDH and FAT.3
Cushing’s disease diminishes or completely negates the negative feedback loop because the cortisol concentration in the body is always high. If the patient has PDH, the negative feedback loop is diminished resulting in a slight decrease in the 4- or 8-hour cortisol levels compared to the baseline concentration. In patients with FATs, the negative feedback loop is completely absent, resulting in no decrease of cortisol in either of the post samples.4 Therefore, two different criteria can be used to diagnose PDH. Either the 4-hour result is <1.4 mcg/dL, or the 4- or 8-hour result is <50% of the baseline cortisol concentration. Up to 35% of dogs with PDH do not fulfill at least one of these criteria, so not meeting these criteria does not automatically diagnose a FAT. If none of the criteria for PDH is met, additional diagnostics must be performed; these may include an abdominal ultrasound to locate an adrenal tumor, a high-dose dexamethasone suppression test, and/or an endogenous ACTH.
High-Dose Dexamethasone Suppression Test, Endogenous ACTH
An HDDST is performed similarly to an LDDST however the dose of dexamethasone is higher at 0.1 mg/kg IV. This test may identify 15% more dogs with PDH than an LDDST.1 Occasionally, the negative feedback loop in dogs with PDH is more resistant and may require a higher dose of dexamethasone to lower the cortisol levels. If the cortisol concentration remains high after an HDDST, then FAT is highly likely.
Endogenous ACTH is the concentration of ACTH naturally produced in the body. Typically, a patient with PDH will have an increased concentration of ACTH in their system, and a patient with FATs will have a decreased concentration of ACTH.4 This test is limited by the fact that certain cases of Cushing’s disease may have ACTH levels in the normal range.1 It is also difficult to collect and process these samples. Samples are obtained using an EDTA tube, centrifuging the sample immediately, separating the EDTA plasma from the red blood cells, and freezing the sample. This must be shipped frozen and cannot arrive more than partially thawed. This test is not diagnostic for Cushing’s disease and is only used to differentiate between PDH and FAT.
Treatment and Monitoring
Multiple treatment approaches can be used, with medical therapy being the most common. Surgical removal of the affected adrenal gland is the treatment of choice in FATs, however, a small number of cases have inoperable tumors.1 In these cases, mitotane can be used for selective adrenocorticolysis, however, this medication can potentially cause complete adrenocorticolysis resulting in iatrogenic hypoadrenocorticism.
Trilostane is a medication that inhibits the synthesis of 3-beta-hydroxysteroid dehydrogenase in the adrenal cortex. This decreases the production of glucocorticoids, with minimal effect on the production of mineralocorticoids.2 This inhibition is reversible with the discontinuation of trilostane. Trilostane is the medication of choice in cases of PDH, however, for FATs it can improve quality of life but does not affect tumor size. Trilostane is given at a starting dose of 1-2 mg/kg PO BID with food.5 It is recommended to repeat an exam, chemistry panel, and an ACTH stim 10 to 14 days after starting this medication or after any dosage change. An ACTH stim should then be performed at months 1, 3, and every 3 months thereafter.1
An ACTH stim is the gold standard test for monitoring Cushing’s disease.2 This test should be performed 4-6 hours after the patient receives trilostane. Post-ACTH cortisol concentrations should optimally be between 1.45 – 9.1 mcg/dL.7 Recently, there have been studies comparing other methods of monitoring with an ACTH stim. The first method was tested in the UK when there was a national shortage of synthetic ACTH. Results indicated that a resting cortisol run on a pre-trilostane sample taken right before the next dose of trilostane was due correlated better with clinical signs than a post-trilostane and/or a post-ACTH cortisol concentration.5 It is recommended that the pre-trilostane cortisol concentration be between 1.5 – 5 mcg/dL for optimal control.5
There have also been studies evaluating 3-hour post-trilostane resting cortisol levels. It has been shown that the cortisol nadir in dogs is 3 hours after receiving trilostane, showing that a 3-hour post-trilostane resting cortisol is the most accurate representation of cortisol concentration.6 Regardless of which protocol is used, a pre-trilostane resting cortisol and a 3-hour post-trilostane resting cortisol should only be used on clinically well dogs. Dogs exhibiting signs of hypocortisolemia, including anorexia, vomiting, and diarrhea, should be fully evaluated using an ACTH stim.5 Further studies are required to determine the best way to monitor Cushing’s disease, but all monitoring tests should also be evaluated in conjunction with the wellbeing of the patient and clinical signs.
References
1. Merrill, Linda, et al. Hyperadrenocorticism: Cushing’s Disease. Small Animal Internal Medicine for Veterinary Technicians and Nurses, Wiley-Blackwell, Ames, IA, 2012, pp. 26–29.
2. Boatright, VMD, Kate. How to Manage Cushing’s Syndrome. DVM 360, MJH Life Sciences, 15 Nov. 2021, www.dvm360.com/view/how-to-manage-cushing-s-syndrome.
3. Diagnostic Testing and Monitoring. AAHA, 2023, www.aaha.org/aaha-guidelines/2023-aaha-selected-endocrinopathies-of-dogs-and-cats-guidelines/canine-hypercortisolism-cushings-syndrome/diagnostic-testing-and-monitoring/.
4. Weir, Malcolm, et al. Cushing’s Disease – Testing: VCA Animal Hospitals. Vca, vcahospitals.com/know-your-pet/cushings-disease-testing. Accessed 14 Dec. 2023.
5. Fletcher, Jon M. Trilostane Treatment and Monitoring: Is the ACTH Stimulation Test Gone for Good? ISVMA.org, Accessed 12 Dec. 2023.
6. Macfarlane, L., et al. Pre-Trilostane and Three-Hour Post-Trilostane Cortisol to Monitor Trilostane Therapy in Dogs. PubMed Central, 4 Nov. 2016, Accessed Dec. 2023.
7. Monitoring Cushing’s. www.dechra-us.com/management-areas/companion-animals/endocrinology/canine-hyperadrenocorticism/monitoring-cushings. Accessed Dec. 2023.
*Please note the opinions in this blog are the expressed opinion of the author(s), and not directly endorsed by VETgirl.
Only VETgirl members can leave comments. Sign In or Join VETgirl now!



the 3 hour post trilostane is a great option for those owners that cannot get here first thing in the morning.