June 2024
In this VETgirl online veterinary continuing education blog, Amanda M. Shelby, RVTg, VTS (Anesthesia/Analgesia) reviews the importance of heart rate and rhythm during general anesthesia in our veterinary patients. Whether you’re a small animal or large animal veterinarian or veterinary technician, you’ll want to read more to learn about the importance of heart rate’s effect on cardiac output!
Matters of the Heart: Importance of Heart Rate and Rhythm During Anesthesia
By Amanda M. Shelby, RVTg, VTS (Anesthesia/Analgesia)
The body is a complex network of systems working in tandem to optimize survival. In sedated or anesthetized patients, monitoring of the cardiopulmonary systems is paramount. The pulmonary system functions optimally to provide ventilation (i.e., elimination of carbon dioxide) and oxygenation (i.e., oxygen saturation of blood) while the cardiovascular system provides circulation—movement of blood through the body. Working optimally, the cardiopulmonary systems provide perfusion, the delivery of oxygen to tissues. Perfusion is challenging to directly measure in clinical settings. Subjectively, capillary refill time and mucous membrane color provide indications of perfusion and oxygenation. Objective methods of monitoring oxygenation, ventilation and circulation are provided in Table 1. Regardless, ensuring adequate perfusion to the tissues is a primary goal of patient monitoring and assessment, in conscious or unconscious patients.

Table 1. Monitoring Methods; Table Courtesy of Amanda Shelby, RVTg, VTS (Anesthesia & Analgesia)
How Does the Heart Rate Affect Perfusion?
Heart rate is just one variable that influences the adequacy of cardiovascular circulation (Figure 1). A common reference range for canine heart rates is 60 – 160 beats per minute; however, this wide range of heart rates fails to ensure adequate perfusion across all canine patients in various clinical situations.(1) The heart rate and rhythm in tandem influence optimal stroke volume and cardiac output. Coupled with systemic vascular resistance, blood pressure is measured to aid in the assessment of patient well-being. When heart rate increases excessively, stroke volume is compromised resulting in decreased cardiac output and potentially low blood pressure. Inversely, low heart rates may decrease cardiac output resulting in low blood pressure when there is reduced systemic vascular resistance.

Figure 1. Cardiovascular Circulation; Figure Courtesy of Amanda M. Shelby, RVTg, VTS (Anesthesia/Analgesia)
Does Normal Blood Pressure Equal Adequate Perfusion?
The assumption commonly made is that patients with normal blood pressure (i.e., systolic arterial pressure [SAP] over 90-160 mmHg, mean arterial pressure [MAP] over 60-80 mmHg) have adequate perfusion.(1) Adequate blood pressure does not always ensure adequate perfusion. In states of excessive vasoconstriction, an increase in systemic vascular resistance occurs and low SpO2 values from the pulse oximeter are common. This demonstrates vasoconstriction could result in decreased perfusion. Conversely, excessive vasodilation resulting in decreased afterload, reduced stroke volume without a compensatory increase in heart rate can also produce a state of low blood pressure and reduced perfusion. However, some reduction in systemic vascular resistance could increase blood flow to tissues, increasing perfusion. Blood pressure is often viewed as a quantitative variable, obtainable in clinical situations. However, given the many variables iidentified in Figure 1 that influence blood pressure, a qualitative approach using the data collected from the whole patient assessment requires interpretation by a dedicated, trained anesthetist to make conclusions on perfusion.
Effect of Heart Rate & Rhythm on Blood Pressure
The heart is a smart organ. Baroreceptors present in the heart respond to changes in variables within the Figure 1 equation. For example, in states of hypotension resulting from hypovolemia (i.e, reduced afterload and preload), the heart rate increases to increase cardiac output and maintain blood pressure—think about patients in hypovolemic shock. The heart’s electrical rhythm influences its mechanical function. Arrhythmias are disruptions in the electrical pathway with or without heart rate abnormality. During arrhythmias patients are at increased risk for reduced cardiac contractility, cardiac output, blood pressure, and potential perfusion. As the heart rate increases, the phase of diastole is minimized. When diastole is shortened, perfusion to the myocardium, ventricular filling, and resulting stroke volume during systole are reduced. This decreased cardiac output because of tachycardia (high heart rates), with or without a tachyarrhythmia, contributes to hypotension and potentially poor perfusion. Similarly, bradycardia (low heart rates), with or without bradyarrhythmias, can also result in decreased cardiac output and blood pressure. Figure 2 demonstrates the relationship of bradyarrhythmia impact on blood pressure in a cat.

Figure 2. Impact of Bradyarrhythmia on Blood Pressure
Heart Rate & Anesthetic Drugs
Most drugs used in the peri-anesthetic period have a dose-dependent effect on heart rate. Table 2 details common peri-anesthetic drugs and their effect on cardiovascular variables seen in Figure 1. As heart rate increases so does myocardial oxygen consumption, along with the incidence of tachyarrhythmias. Extreme increases in heart rate decrease ventricular filling time and stroke volume resulting in decreased cardiac output and blood pressure. Figure 3 is a video that shows a patient in a tachyarrhythmia with resulting pulse pressure variance on the arterial waveform and plethysmograph. Although not hypotensive, stroke volume for some of the cardiac contractions is compromised. Anticholinergics increase heart rate and as a result, increase cardiac output and blood pressure.
Conversely, most opioids cause bradycardia. When bradycardia is excessive, cardiac output decreases resulting in reduced blood pressure. Buprenorphine, a partial mu opioid agonist, does not have profound cardiovascular effects at clinical doses. Alpha2 adrenergic agonists cause a reduction in heart rate as a reflex response to an increase in systemic vascular resistance, vasoconstriction. While blood pressure increases due to vasoconstriction, perfusion often decreases. When alpha2 adrenergic agonists are used as premedication agent prior to halogenated inhalants, which cause a decrease in contractility and vasodilation, and opioids, which augment bradycardia, this results in a reduced cardiac output and hypotension. Acepromazine causes a reduction in systemic vascular resistance and a resulting decrease in blood pressure with a potential increase in perfusion. In combination with other peri-anesthetic drugs, hypotension could result. The important concept to recognize is that blood pressure and perfusion do not have a linear relationship.

Table 2. Common Peri-Anesthetic Drugs Use in Cats and Dogs on Cardiovascular Parameters. Table courtesy of Amanda M. Shelby, RVTg, VTS (Anesthesia & Analgesia)
What is the ‘Ideal’ Heart Rate Under Anesthesia?
The ideal heart rate under anesthesia for dogs and cats is a heart rate that maintains blood pressure and optimizes tissue perfusion. The author prefers to perform a pre-anesthetic assessment of each patient to identify the patient’s specific resting heart rate and blood pressure prior to the administration of any peri-anesthetics, when possible, to maintain a heart rate within 20-30% of the patient’s specific resting heart rate. With the use of alpha2 adrenergic agonists, this general guideline often requires allowances for heart rates lower than 20-30% less than the patient’s specific resting heart rate. When this occurs, blood pressure is used to assist the anesthetist in determining if the heart rate requires a treatment response. If a patient experiences hypotension with a low heart rate, an anticholinergic may be used to increase heart rate and cardiac output resulting in improved blood pressure. Conversely, when bradycardia is associated with hypertension because of administration of an alpha2 adrenergic agonist, treatment is often not warranted. When tachycardia with hypotension under anesthesia is experienced, identifying the contributing cause of hypotension is prioritized. Rarely does the tachycardia require direct treatment with a beta blocker or calcium channel blocker. Regardless of brady- or tachycardia, electrocardiographic (ECG) evaluation should be performed. Heart rates with accompanying dysrhythmias often have a negative impact on cardiac output, blood pressure, and perfusion. With arrhythmias, priority is given to identification of the arrhythmia, resolving the underlying cause, and returning to normal electrical rhythm and rate.
What About Cats?
Unlike dogs, domesticated cats are relatively similar in size and metabolic rate. This minimizes variation in accepted normal ranges. Slight variations in reference manuals exist but the normal heart rate in cats is 100-250 bpm.(1) Bradycardia in cats has been identified as heart rates under 100 bpm. (1) Tachycardias have been identified over 250 bpm.(1) While species variation in response to peri-anesthetic drugs do exist, target blood pressure values for cats are comparable to dogs. Like dogs, evaluating the whole patient prior to the administration of peri-anesthetics is ideal. While not always possible in cats, evaluating heart rate with blood pressure and tissue perfusion in the context of the patient’s physical examination history aides the veterinary professional in identification of heart rate and rhythm disturbances that could result in increased morbidity and mortality.
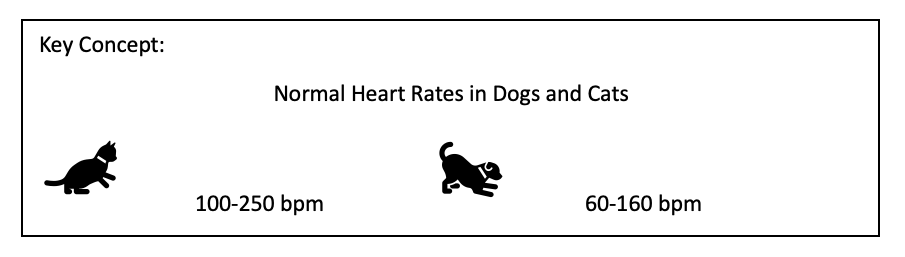
Figure courtesy of Amanda M. Shelby, RVTg, VTS (Anesthesia/Analgesia)
Summary
Heart rate is one of the measurable variables veterinary professionals can use to assess the cardiovascular system. In conjunction with arterial blood pressure and subjective means of evaluating perfusion (i.e., capillary refill time, mucous membrane color), ensuring a normal heart rate and rhythm helps ensure the cardiovascular system is working optimally. Additionally, in anesthetized patients using heart rate, rhythm, and blood pressure to evaluate circulation, along with the use of pulse oximetry to evaluate oxygenation and capnography to assist in the evaluation of ventilation, by a dedicated, trained veterinary professional can optimize patient outcomes.
References:
1. Shelby AM, McKune CM. Small Animal Anesthesia Techniques. 2 ed. Hoboken, NJ: John Wiley & Sons, Inc.; 2023.
2. Muir W. Cardiovascular System. In: Tranquilli W, Thurmon J, Grimm K, editors. Lumb & Jones’ Veterinary Anesthesia and Analgesia. Ames, IA: Blackwell Publishing; 2007. p. 61-116.
3. Greene SA, Hartsfield SM, Tyner CL. Cardiovascular effects of butorphanol in halothane-anesthetized dogs. Am J Vet Res 1990;51(8):1276-9.
4. Farver TB, Haskins SC, Patz JD. Cardiopulmonary effects of acepromazine and of the subsequent administration of ketamine in the dog. Am J Vet Res 1986;47(3):631-5.
5. Pagel PS, Hettrick DA, Kersten JR, et al. Dexmedetomidine produces similar alterations in the determinants of left ventricular afterload in conscious dogs before and after the development of pacing-induced cardiomyopathy. Anesthesiology 1998;89(3):741-8.
6. Henao-Guerrero N, Riccó CH. Comparison of the cardiorespiratory effects of a combination of ketamine and propofol, propofol alone, or a combination of ketamine and diazepam before and after induction of anesthesia in dogs sedated with acepromazine and oxymorphone. Am J Vet Res 2014;75(3):231-9.
7. Muir W, Lerche P, Wiese A, et al. Cardiorespiratory and anesthetic effects of clinical and supraclinical doses of alfaxalone in dogs. Vet Anaesth Analg 2008;35(6):451-62.
8. Muir W, Lerche P, Wiese A, et al. The cardiorespiratory and anesthetic effects of clinical and supraclinical doses of alfaxalone in cats. Veterinary Anaesthesia and Analgesia 2009;36(1):42-54.
9. Rodríguez JM, Muñoz-Rascón P, Navarrete-Calvo R, et al. Comparison of the cardiopulmonary parameters after induction of anaesthesia with alphaxalone or etomidate in dogs. Veterinary Anaesthesia and Analgesia 2012;39(4):357-65.
Please note the opinions in this blog are the expressed opinion of the author(s)/sponsor, and not directly endorsed by VETgirl.
Only VETgirl members can leave comments. Sign In or Join VETgirl now!
Great information!
Thanks so much for this!